Medical benefits patients have 1.87 times higher risk of death during abdominal aortic aneurysm stenting
Aug 27, 2025
|
Professor Oh Se-jin of Cardiovascular Thoracic Surgery at Boramae Hospital in Seoul, operated by Seoul National University Hospital, Professor Jang Won-mo of the Department of Public Medicine, and Dr. Choi Hong-jae of Cardiovascular Thoracic Surgery published the results of a study that analyzed the prognosis of 15,065 abdominal aortic aneurysms from 2002 to 2019 using big data from the National Health Insurance Service.
Abdominal aortic aneurysm is a disease that accompanies the risk of rupture due to abnormal expansion of the abdominal aortic wall, and is treated with open surgery (OAR) or intravascular stent insertion (EVAR). The mortality rate in rupture is very high, so early diagnosis and appropriate treatment are important.
The patient's prognosis is greatly influenced by socioeconomic factors such as access to medical services as well as health conditions and comorbidities. Overseas studies have reported that low-income patients have an approximately 46% higher risk of postoperative death, and this study confirmed this gap with large-scale domestic data.
The research team compared 15,065 abdominal aortic aneurysm surgery patients with 2,753 laparotomy patients with 12,312 stent implantation patients. By type of insurance, 14,065 health insurance and 1,000 medical benefits were counted, and the proportion of patients with stent implantation was 81.3% for health insurance and 87.8% for medical benefits
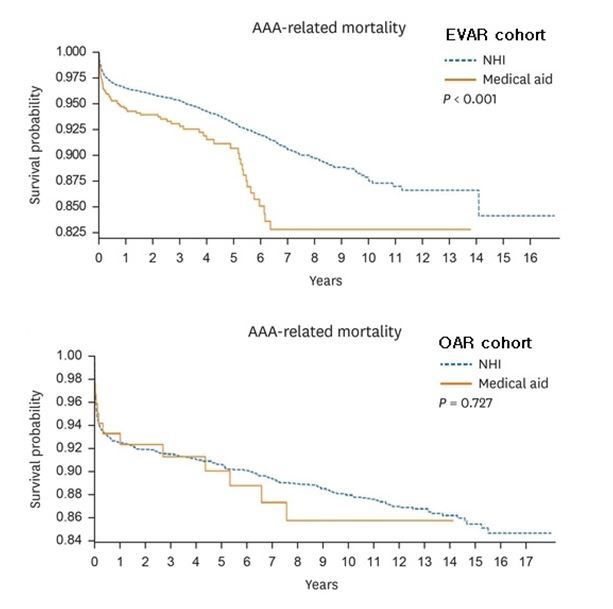
In the main results, the prognosis of the stent implantation patient group was clear according to the type of insurance. The abdominal aortic aneurysm associated mortality rate in medical benefit patients was significantly higher than that in health insurance patients, and the risk of mortality in medical benefit patients was approximately 1.87 times in multivariate analysis (P<0.001). On the other hand, in the laparotomy patient group, the difference in abdominal aortic aneurysm-related mortality according to insurance type was not significant (P=0.727)
This study is significant in that it is a long-term follow-up study that encompasses both open surgery (OAR) and intravascular stent implantation (EVAR) based on domestic data, unlike the existing short-term analysis focused on Western-centered, elderly Medicare subscribers and single surgery. In particular, it reflected the actual clinical site more precisely, including the entire patient population who underwent the operation in Korea.
In particular, the vulnerable group of abdominal aortic aneurysms often undergo laparotomy due to patient characteristics and high surgical costs around the world, but in Korea, as the national medical insurance system is applied, a unique pattern has been observed in which intravascular stent insertion is performed more often in medical benefit patients.
The research team emphasized that the results show that socioeconomic factors actually affect the prognosis of surgery in patients with abdominal aortic aneurysms, rather than simply differences or stability in surgical methods.
It is expected to be an important basis for contributing to the improvement of health care based on equity in the future, suggesting the need to strengthen postoperative follow-up management and treatment strategies for vulnerable patients, while identifying the impact of socioeconomic gaps on actual medical outcomes.
Professor Oh Se-jin said, "This study goes beyond just the difference in insurance type, and shows that socioeconomic factors are acting complexly on the prognosis of patients with abdominal aortic aneurysm."Postoperative management and institutional supplementation should be discussed together to improve the prognosis of abdominal aortic aneurysm in patients with medical vulnerability." he said.
The results of this study were recently published in the online edition of the official journal of the Korean Medical Science.
|
This article was translated by Naver AI translator.