Will advanced hepatocellular carcinoma open up the possibility of liver resection and liver transplantation conversion…The First Examination of Systemic Immuno-Cancer Treatment Effect
Sep 17, 2025
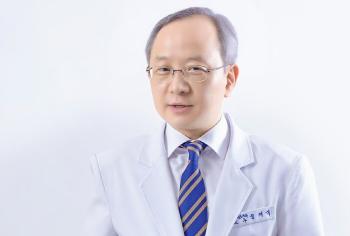
A research team led by Professor Jeon Hong-jae (co-communication) and Professor Kim Jung-sun (co-author) of the Oncology Department of Oncology at Bundang Cha Hospital (Director Yoon Sang-wook) of Cha Medical University and Professor Jeong-sun (co-author) revealed the results of a study that suggested the possibility of combination therapy of atezolizumab and bevacizumab (AB) 'Conversion Therapy'. This study is the result of a large-scale international joint study conducted in cooperation with 48 medical institutions around the world, including the United States, Italy, and Japan, and was published in the latest issue of the prestigious journal River Cancer in the field of liver cancer.
Healing conversion therapy is a method of first performing chemotherapy on patients whose cancer has progressed too much to be operated or transplanted, reducing the size of the tumor, and then continuing it to radical treatments such as liver transplantation or liver replacement drugs (treatment aimed at healing). This means that if a patient who was not subject to surgery responds well to chemotherapy, he or she will have an opportunity for a surgical cure.
This study is the world's largest data-based study that analyzed the possibility of therapeutic conversion therapy in 2,379 patients with hepatocellular carcinoma by comparing atezolizumab with bevacizumab (AB) combination therapy and renbatinib (LENV), which are widely used as first-line treatments.
The research team focused on whether patients who were initially unable to operate or transplant could be converted to radical treatments such as liver resection or liver transplantation due to reduced cancer after chemotherapy. As a result, the response rate of atezolizumab and bevacizumab combination therapy was 29%, higher than that of renbatinib 24%. In addition, the conversion potential was 16%, higher than that of renbatinib 13%. In particular, the 3-year survival rate of patients who received curative treatment after the combination therapy of atezolizumab and bevacizumab was 93%, showing that immuno-oncology drugs can contribute to long-term survival.
However, the actual conversion rate was low at 3% in both groups, highlighting the importance of treatment infrastructure such as patient selection process, multidisciplinary treatment, and liver transplantation programs. The research team defined it as such an under-conversion and emphasized the need to improve treatment strategies in the future.
Professor Hong-jae Jeon said, "This study is the first international study to investigate the possibility that systemic immuno-cancer treatment can lead to radical treatment in patients with advanced hepatocellular carcinoma. In the future, we will be able to provide radical opportunities to more patients by strengthening patient-specific treatment strategies and multidisciplinary cooperation."
This study was conducted with basic research support from the Ministry of Science and ICT and the Korea Research Foundation.
Healing conversion therapy is a method of first performing chemotherapy on patients whose cancer has progressed too much to be operated or transplanted, reducing the size of the tumor, and then continuing it to radical treatments such as liver transplantation or liver replacement drugs (treatment aimed at healing). This means that if a patient who was not subject to surgery responds well to chemotherapy, he or she will have an opportunity for a surgical cure.
This study is the world's largest data-based study that analyzed the possibility of therapeutic conversion therapy in 2,379 patients with hepatocellular carcinoma by comparing atezolizumab with bevacizumab (AB) combination therapy and renbatinib (LENV), which are widely used as first-line treatments.
The research team focused on whether patients who were initially unable to operate or transplant could be converted to radical treatments such as liver resection or liver transplantation due to reduced cancer after chemotherapy. As a result, the response rate of atezolizumab and bevacizumab combination therapy was 29%, higher than that of renbatinib 24%. In addition, the conversion potential was 16%, higher than that of renbatinib 13%. In particular, the 3-year survival rate of patients who received curative treatment after the combination therapy of atezolizumab and bevacizumab was 93%, showing that immuno-oncology drugs can contribute to long-term survival.
However, the actual conversion rate was low at 3% in both groups, highlighting the importance of treatment infrastructure such as patient selection process, multidisciplinary treatment, and liver transplantation programs. The research team defined it as such an under-conversion and emphasized the need to improve treatment strategies in the future.
Professor Hong-jae Jeon said, "This study is the first international study to investigate the possibility that systemic immuno-cancer treatment can lead to radical treatment in patients with advanced hepatocellular carcinoma. In the future, we will be able to provide radical opportunities to more patients by strengthening patient-specific treatment strategies and multidisciplinary cooperation."
This study was conducted with basic research support from the Ministry of Science and ICT and the Korea Research Foundation.
|
This article was translated by Naver AI translator.