Hepatitis B Patients' Liver Cancer Prediction, Development of a New Model...82% accuracy
Oct 29, 2025
|
A research team led by Kim Seung-up, a professor of gastroenterology at Yonsei University's Medical Center Severance Hospital, and Jeon Hye-yeon, a professor of gastroenterology at Yongin Severance Hospital, announced on the 29th that the predictive model, which combines the existing aMAP score with the measurement of liver stiffness, can accurately predict the risk of liver cancer and reach 82%.
The results of the study, which included five advanced general hospitals, including Korea University Medical School, Soonchunhyang University Medical School, and Hong Kong Chinese Medical School, were published in the international journal 『Clinical Gastroenterology and Heptology』.
Hepatitis B, one of the common liver diseases in Korea, is considered a major cause of liver cancer worldwide. In Korea, where most vertical infections from the mother occur, most of them progress to chronic conditions and can worsen into cirrhosis or liver cancer. In particular, liver fibrosis, which remains after antiviral therapy, acts as a key risk factor for the development of liver cancer.
The existing evaluation of liver fibrosis was conducted by liver biopsy as a standard. However, due to the cost of testing, complications, and differences between examiners, there are some restrictions on its use in predicting and diagnosing liver cancer, so non-invasive testing has recently attracted attention as an alternative.
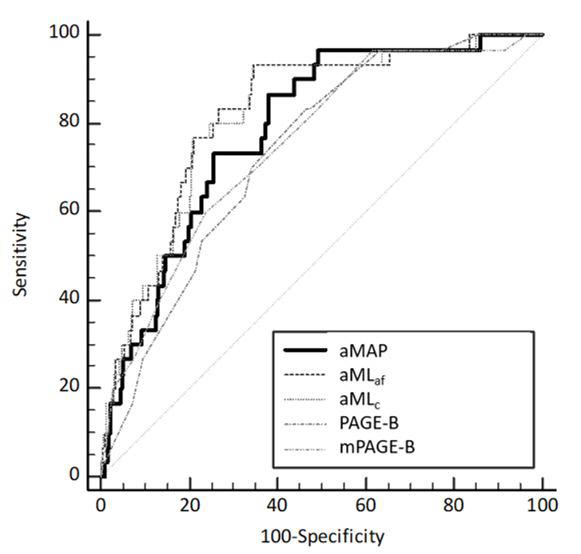
The research team developed a new predictive model that combines aMAP score and a measurement of liver stiffness (LS). The aMAP score is a risk predictor based on age, sex, serum albumin, bilirubin, and platelet count. In addition, the measurement of liver stiffness (LS) using instantaneous elasticity measurement (VCTE) was combined to reflect the risk of residual fibrosis. There are two predictive models developed to reflect cirrhosis stiffness: aMLaf based on advanced fibrosis and aMLc based on cirrhosis.
The research team analyzed the accuracy of the new predictive model with an average follow-up of more than 5 years in 944 patients with chronic hepatitis B who started antiviral therapy from May 2005 to July 2021. Comparisons were made with the liver cancer prediction models proposed by the existing European Liver Society, 'PAGE-B', 'mPAGE-B'.
As a result of the analysis, both aMLaf and aMLc predictive models showed superior predictive performance compared to the existing PAGE-B and mPAGE-B models. The AUROC value, which represents the accuracy of the prediction of liver cancer after 5 years in hepatitis B patients, was 0.82 (82%) in both models, statistically significantly ahead of the conventional models (PAEG-B (0.74) and mPAGE-B (0.75). In particular, there was no occurrence of liver cancer during the follow-up period in the aMLaf low-risk group.
In addition, the research team also performed well in the Hong Kong Chinese Medical School cohort analysis of 61 hepatitis B patients, with aMAP score and cirrhosis measurement combined with more than 80% predictive accuracy.
Professor Kim Seung-up "This study confirmed that the combination of aMAP score and cirrhosis measurements can provide a more precise assessment of the risk of liver cancer in chronic hepatitis B patients" Professor Hye-yeon Jeon said "The new prediction model will be able to clearly distinguish low-risk groups, reducing the unnecessary burden of testing and creating a more aggressive customized monitoring strategy for high-risk groups."
|
This article was translated by Naver AI translator.