Progressive cancer patients find out for the first time in the world that the use of broad-spectrum antibiotics surged three months before their death
Oct 29, 2025
|
A joint research team led by Professor Yoo Shin-hye of Seoul National University Hospital, Professor Kim Jung-han of Ewha Mokdong Hospital, and Professor Shim Jin-ah of Hallym University (researcher Yoo Ji-won) announced on the 29th that they analyzed the use of broad-spectrum antibiotics in advanced cancer patients for six months before their death based on data from the Health Insurance Corporation of 515,000 people collected from 2002 to 2021.
Patients with advanced cancer are frequently prescribed broad-spectrum antibiotics as their immunity decreases and the risk of infection increases toward the end of the year. However, even if there is no actual infection, it is often administered only with fever or inflammation levels. Frequent broad-spectrum antibiotic use increases the risk of side effects, secondary infections, and resistant bacteria, which may not only add to physical pain but also cause a vicious cycle that requires more intense antibiotic treatment.
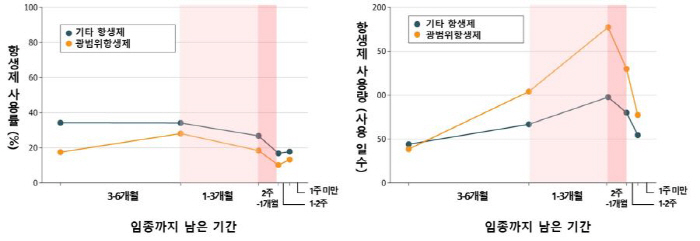
The research team divided the six months before the death of advanced cancer patients into five sections (one week, one to two weeks, two to one month, one to three months, and three to six months), and then analyzed the use and use of four broad-spectrum antibiotics (penicillin, cephalosporin, carbapenem, and glycopeptide). The rate of use was measured by the proportion of patients who used broad-spectrum antibiotics more than once, and usage was measured by the number of days of broad-spectrum antibiotic use during the entire hospitalization period per 1,000 patients.
As a result of the analysis, more than half (55.9%) of all patients used broad-spectrum antibiotics in the 6 months before death. In particular, the usage rate was highest in '1 to 3 months prior to termination' and usage was '2 weeks to 1 month prior to termination', respectively.
In addition, in the analysis by carcinoma, blood cancer patients (non-Hodgkin's lymphoma, leukemia, multiple myeloma) had higher use and use of broad-spectrum antibiotics for six months before death than solid cancer patients (lung cancer, liver cancer, stomach cancer, colon cancer, pancreatic cancer, prostate cancer, gallbladder and biliary cancer, and breast cancer). In particular, leukemia patients had 1.5 times higher use rate and 1.21 times higher use right before death than lung cancer patients who frequently use wide-range antibiotics among solid cancers.
These results show a tendency for broad-spectrum antibiotic therapy to be specifically focused on '3 months to 2 weeks prior to end-of-life as the patient's physical function rapidly deteriorates and the frequency of hospitalization increases. The research team emphasized the importance of minimizing the use of unnecessary broad-spectrum antibiotics through 'palliative care', which supports decision-making tailored to the patient's values and care goals, along with appropriate antibiotic treatment.
Professor Yoo Shin-hye (SNU Hospital palliative care and clinical ethics center, corresponding author) "This study is the first in the world to investigate the use of broad-spectrum antibiotics at the end of life in advanced cancer patients, and is expected to serve as the basis for future antibiotic use guidelines and palliative care policies."
Professor Kim Jung-han (1 author, infectious medicine department at Lee Daemok-dong Hospital) said "It is reasonable to use broad-spectrum antibiotics if the benefits are clear even in patients in their late life, but unnecessary use requires sufficient discussion to cause side effects and increase the risk of developing multidrug-resistant bacteria, thereby interfering with dignified death."
The study was conducted with the support of the Ministry of Health and Welfare 'Patient-centered Medical Technology Optimization Research Project' and was published in the recent issue of the American Medical Association Journal 'JAMA Network Open (IF:13.8)'.
|
This article was translated by Naver AI translator.