Measuring the degree of liver cancer immune cell exhaustion and predicting the effectiveness of immune anticancer drugs
Nov 10, 2025
|
Recently, PD-1 immune checkpoint inhibitors, which are immune anticancer drugs that restore immune cell function, have been widely introduced into clinical practice, but the treatment effect varies greatly from patient to patient, so understanding of the tumor immune microenvironment has been considered an urgent task.
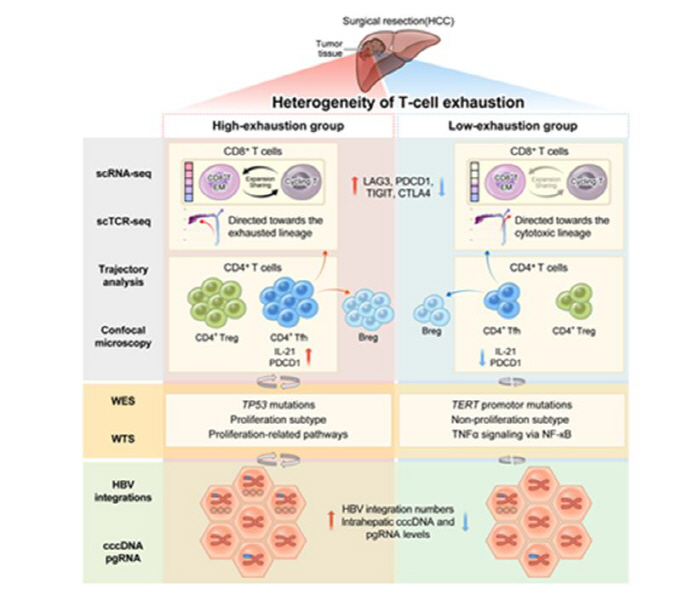
The research team performed multiple omics analysis, including single-cell RNA sequencing, full-length exome sequencing, and full-length transcriptome sequencing, on eight patients who underwent liver cancer surgery at Seoul St. Mary's Hospital. Through this, the patients were classified into the immune high-fatigue group (2) and the low-fatigue group (6), and as a result, it was confirmed that even patients diagnosed with liver cancer had distinct differences in the biological characteristics of cancer depending on the degree to which immune cells were exhausted.
Three key characteristics were identified in the patients' liver, depending on whether immune cells were exhausted or not.
First, abnormal proliferation of immune cells was prominent as the first feature. The degree of immune cell clone expansion in the high-fatigue group was 1.7 times higher than that of the low-fatigue group with a Gini coefficient of 0.83, and it showed that certain immune cells proliferated excessively and differentiated into several forms. In addition, CD4+-regulated T cells that inhibit immune function and PDCD1 gene expression that transmits immunosuppressive signals also increased, resulting in immune cells losing their ability to attack cancer cells.
As a second feature, the pattern of genetic variation was also different. The hypertrophic group showed a high mutation rate of TP53, a cancer suppressor gene, and a proliferative subtype characteristic in which cancer cells proliferated rapidly. On the other hand, the low-fatigue group mainly shows TERT gene mutations that contribute to cancer development by allowing cells to continuously divide, and it was confirmed that cancer occurs through completely different gene mutations between the high-fatigue group and the low-fatigue group.
Finally, the degree of penetration of hepatitis B virus was significantly different. Comparing the two patient groups, high levels of covalent cyclic DNA and pregenomic RNA, which are viral reservoirs in the liver, were high in the high-fatigue group, and many S-convergence transcripts, abnormal RNAs in which the S gene that makes the surface protein of hepatitis B virus is fused with human genes, were found. This convincingly proves the model that the more severe immune cell exhaustion, the more virus integration, which in turn creates a vicious cycle structure that increases the likelihood of carcinogenesis.
To verify this, the research team further analyzed a cohort of 106 independent hepatitis B-related liver cancer patients (28 high and 78 low) and observed the same phenomenon in the verification cohort, proving that the finding is a reproducible phenomenon.
Professor Lee Soon-kyu, the first author of the study, found that even with the same liver cancer, each patient has a different tumor immune microenvironment, and the genetic mutation pattern and the degree of virus integration differ depending on the degree of exhaustion of T cells" he explained the meaning of the study.
Professor Jang Jeong-won, the corresponding author, explained that "T cell exhaustion is a major cause of lowering the effectiveness of immune cancer treatment, so this study will be an important basis for accurately evaluating the patient's immune exhaustion status and establishing a customized treatment strategy.".
Meanwhile, liver cancer is the third leading cause of cancer death worldwide and is a fatal disease with a 5-year survival rate of only about 18%, and more than 60-70% of liver cancer patients in Korea are known to be related to hepatitis B virus infection. This study is expected to have laid the foundation for predicting the response of immuno-cancer drugs and selecting individual customized treatments based on the evaluation of immune exhaustion status of liver cancer patients.
The results of this study were recently published in the international journal 『JHEP Reports" published by the European Liver Association.
|
This article was translated by Naver AI translator.