Pancreatic cancer that is difficult to operate, 3000V electrical therapy is effective...Average survival after electroporation
Mar 11, 2025
|
A team of professors Kim Man-deuk and Kwon Joon-ho of Severance Hospital's radiology department said the average survival period increased by up to 9 months as a result of IRE treatment for 13 pancreatic cancer patients with difficult surgery. Professor Kim Man-deuk will present the clinical results at the Society of Intervention Radiology (SIR) in Nashville, USA, on the 30th.
The 5-year survival rate of pancreatic cancer is only 15.9%. Pancreatic cancer that can be operated is 20% of the total, and most of them are diagnosed as inoperable. In the case of locally advanced pancreatic cancer that invades surrounding blood vessels or organs, the average survival period is about 6 to 11 months after diagnosis, even if chemotherapy is received.
IRE was developed in the United States and is used all over the world. In Korea, it was first introduced to Severance Hospital in 2016 and was recently recognized as a new medical technology.
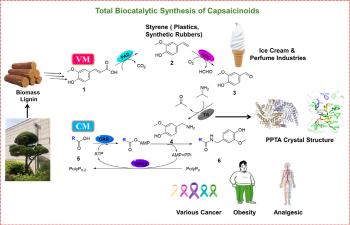
IRE is a treatment that removes cancer cells by inserting three to six electrodes around cancer tissues and flowing high-pressure electricity. It uses 3000V of electricity, which is more than 10 times the voltage of 220V of a household outlet. Because IRE does not utilize heat energy, the surrounding blood vessels or tissues are hardly damaged. High-pressure electricity creates several holes in the membrane of cancer cells that are too fine to be identified with the naked eye, and these micropores break the internal and external balance of the cells, leading to cell death.
In particular, as cancer cells die, cancer cell materials are exposed through microholes, which act like vaccines and promote immune cell activity in the body.
Professor Kim Man-deuk's team performed IRE treatment on 13 pancreatic cancer patients who could not operate. As a result, the average survival period after the procedure of the patient was 20.7 months, an increase of up to 9 months from 11 to 14 months (existing IRE procedures). The average survival period after diagnosis increased from 17 to 27 months (existing IRE procedures) to an average of 43.9 months, up to 26 months.
Compared to previously reported IRE treatment, this clinical result maximizes the effectiveness of the procedure and reduces the procedure time. The IRE equipment used this time is an EPO system developed by The Standard, a domestic medical device company, that maximizes the effectiveness of the procedure and reduces the procedure time compared to the existing IRE equipment.
In the case of existing IRE equipment, three to six electrodes must be inserted in parallel at regular intervals of 1.5 to 2 cm, requiring considerable skill to perform the procedure. However, in the case of an EPO system, three to four small electrodes can be inserted at once as clustered electrodes fixed at regular intervals in one large electrode. As a result of Professor Kim Man-deuk participating in the development of the equipment and discussing the idea with the development team, it was possible to increase the effectiveness of the procedure and reduce the procedure time by more than 50% through multiple electrodes.
The procedure inserts electrodes around cancer tissues through imaging tests such as ultrasound, CT, and vascular imaging after general anesthesia. In the early stages of IRE introduction, it was opened and treated, but recently, it is performed through the skin instead of the open, so the scar is small and you can be discharged in about a week.
Professor Kim Man-deuk said, `If the tumor has spread to other organs or is too large, the IRE treatment indication does not work or the effectiveness decreases.' `Although this study requires further follow-up studies due to the small number of patients, it could be an alternative for patients who cannot operate and have reduced effectiveness of chemotherapy or have no other treatment options due to side effects of chemotherapy.'
|
This article was translated by Naver AI translator.