The longer the osteoporosis treatment is discontinued before extraction, the lower the risk of jawbone necrosis
|
Normal bones remain healthy, balancing 'bone absorption' that removes old or damaged tissue with 'bone formation' that makes new bones. However, the bones of osteoporosis patients gradually become thinner and weaker as bone formation cannot keep up with the rate of bone absorption.
This osteoporosis is treated by suppressing bone absorption to maintain or increase bone density, and a typical drug is injection-type bisphosphonate, which is administered with 'zolidronate (administered once a year, for high-risk groups)' or 'Ibandronate (administered quarterly, for low-risk groups)' depending on the patient's condition.
However, if bone absorption is excessively suppressed, old bones are not well removed and damage is accumulated, which can cause side effects such as jawbone necrosis or atypical femur fractures. In particular, the jawbone is a region with a lot of daily stimulation, and surgical treatment such as extraction and implantation while bone absorption is suppressed is likely to delay recovery and lead to necrosis. Nevertheless, clear clinical guidelines were not in place due to the lack of evidence on when bisphosphonate was discontinued before extraction.
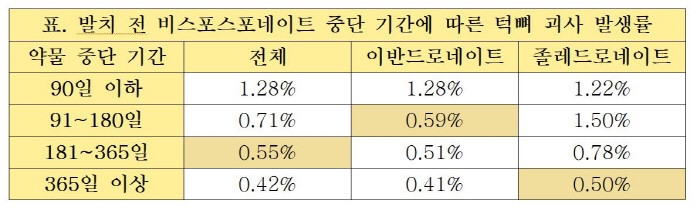
Accordingly, the research team conducted a study to analyze the association between the duration of drug discontinuation before extraction and the risk of jawbone necrosis for patients receiving injectable bisphosphonate treatment among the insurance data of osteoporosis patients. A total of 152,299 patients were compared and analyzed by dividing them into four groups according to the duration of drug discontinuation.
Studies have shown that the risk of developing jawbone necrosis significantly decreases with longer duration of discontinuation of bisphosphonate. The incidence of jawbone necrosis in the group who stopped the drug for less than 90 days was 1.28%, but 0.71% in the group who stopped 91-180 days and 0.42% in the group who stopped for more than 365 days, and the longer the discontinuation period, the lower the incidence of jawbone necrosis by up to three times.
In addition, it was confirmed that there was a difference in the incidence of jawbone necrosis according to the duration of discontinuation by drug type. The incidence of necrosis of isandronate was significantly reduced when only about 91 days or more were stopped, whereas the incidence of necrosis was effectively reduced only when the zoledronate was stopped for more than a year. The research team explained that Zoledronate has a longer half-life and remains in the body for a long time.
Based on the world's largest clinical data, this study is of great significance in that it has demonstrated that the effective timing of discontinuation of injectable bisphosphonate is effective in preventing jawbone necrosis. This can serve as a key basis for establishing safe treatment strategies between osteoporosis treatment and dental treatment, and is expected to provide important guidelines for academic and clinical guidelines.
Professor Gong Sung-hye (1 author) of the Department of Endocrine Metabolism at Seoul National University Bundang Hospital said, "The study found that discontinuation of bisphosphonate may lower the risk of bone necrosis, but on the other hand, the longer the duration of discontinuation, the higher the risk of spinal and hip fractures." "Osteoporosis patients scheduled for dental surgery should consult with a related specialist on whether and when to discontinue drugs."," he added.
Professor Lee Hyo-jung (corresponding author) of Dental Clinic at Seoul National University Bundang Hospital said, `Tuck bone necrosis is a difficult-to-treat and has a big impact on the quality of life, especially in osteoporosis patients. Adjusting the timing of treatment considering the history of drug use will reduce the risk of necrosis.'
Meanwhile, this study was conducted with Professor Park Jung-hyun of Dental Clinic at Ewha Womans University Mokdong Hospital (co-author) and Professor Kim Jin-woo of Dental Clinic at Ewha Womans University Seoul Hospital (co-corresponding author), and was published in the international academic journal SCI(E) 'Nature Communications (IF=16.1)'.
|
This article was translated by Naver AI translator.