Terminal cancer patients with multidrug resistance bacteria use low hospice and high death rates in advanced hospitals
|
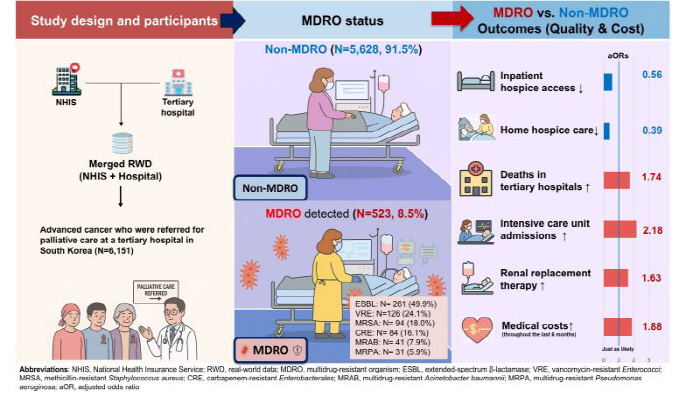
Professor Kim Jeong-han of the Department of Infectious Diseases at Ewha Womans University Mokdong Hospital, Professor Yoo Shin-hye of the Center for palliative care and clinical ethics at Seoul National University, and Professor Shim Jin-ah of the Department of Artificial Intelligence Convergence at Hallym University (researcher Yoo Ji-won) announced on the 1st that they analyzed the medical records of 6,151 terminal cancer patients who received palliative care counseling from 2018 to 2023 and the data from the Health Insurance Corporation.
Based on the timing of palliative care counseling, the research team compared patients who were confirmed to have multidrug-resistant bacteria for the previous six months with those who did not have them and analyzed the frequency of invasive life-sustaining treatment such as ▲ hospice utilization ▲ mortality rate in upper general hospitals ▲ intensive care unit admission, ventilator treatment, and dialysis.
As a result of the analysis, 523 (8.5%) of all patients had multidrug-resistant bacteria, and these patients were significantly less likely to use hospice compared to non-carrying patients. Hospitalized hospice utilization was 24.1%, lower than non-holding patients (37.8%), and home-type hospice utilization was also 2.7%, lower than non-holding patients (7.4%).
On the other hand, the rate of death in advanced general hospitals was about half (46.1%) of patients with multidrug-resistant bacteria, significantly higher than those with non-drug (28.9%). In addition, the rate of receiving invasive life-sustaining treatment such as intensive care unit admission or dialysis was also higher in the holding group, and the burden of medical expenses for 6 months before death also increased significantly in the holding group than in the non-holding group.
Multidrug-resistant bacteria are bacteria that have acquired resistance that is difficult to treat with existing antibiotics, and in Korea, methicillin-resistant Staphylococcus aureus (MRSA), vancomycin-resistant enterobacterium (VRE), carbapenem-resistant Enterobacteriaceae (CRE), multidrug-resistant Pseudomonas aeruginosa (MRPA), and multidrug-resistant Acinetobacter Baumani (MRAB) are included as legal infections. These bacteria are important issues in infection control due to the limited choice of antibiotics and the high risk of transmission in hospitals.
In particular, end-stage cancer patients have decreased immunity and increased risk of infection due to the disease itself and chemotherapy. As a result, frequent inpatient treatment and antibiotic prescriptions are repeated, and the risk of colonization of multidrug-resistant bacteria increases in the process. When multidrug-resistant bacteria are confirmed, strengthened infection control measures such as contactism, isolation, and repeated testing are needed, which can lead to undesirable consequences in terms of quality of life at the end of life, such as limiting interactions with family members and delaying hospice conversion.
The research team emphasized the need for a patient-centered infection control strategy that reflects the trajectory of life of terminally ill cancer patients, saying, "This analysis is the first study to empirically show how infection control policies and multidrug resistant bacteria management affect the treatment path and quality of end-of-life care for terminally ill patients."
Professor Yoo Shin-hye (SNU Hospital palliative care and clinical ethics center, corresponding author) "It is time to consider systematic improvement measures to overcome the restrictions on the use of hospice (such as the burden of quarantine facilities and manpower) in order not to deprive patients with multidrug-resistant bacteria of the opportunity to care." It also requires medical staff-patient-family together decision-making on the use of end-of-life antibiotics beyond just the therapeutic goal of eradicating bacteria.'
Professor Kim Jung-han (Director of Infection Control at Lee Daemok-dong Hospital, 1 author) said, "As the quality of care at the end of life depends greatly on where and how patients and their families will receive the care they want, efforts are needed to reduce the colonization of multidrug-resistant bacteria. It is of utmost importance to carefully decide on the use of systemic antibiotics and strictly follow basic infection control rules such as washing hands.'
Meanwhile, the study was carried out with the support of the Ministry of Health and Welfare 'Patient-centered Medical Technology Optimization Research Project' and was published online in the recent issue of the European Society of Clinical Microbiology and Infection (CMI, Influence Index IF 8.5)'.
|
This article was translated by Naver AI translator.