A Simple Blood Test Suggests Early Diagnosis Of Alzheimer's Disease
Apr 22, 2025
|
Alzheimer's disease is a typical degenerative brain disease that causes memory loss and cognitive decline, and is considered the most common cause of dementia. Early diagnosis and treatment intervention are of paramount importance because irreversible damage to the brain occurs as it progresses.
However, in reality, many patients are diagnosed only after the disease has progressed considerably. This is because the burden of testing required for diagnosis is high. Currently, widely performed PET (positron emission tomography) tests are expensive, and cerebrospinal fluid tests are invasive to insert needles into the lumbar spine after anesthesia, making both tests difficult to use on a daily basis.
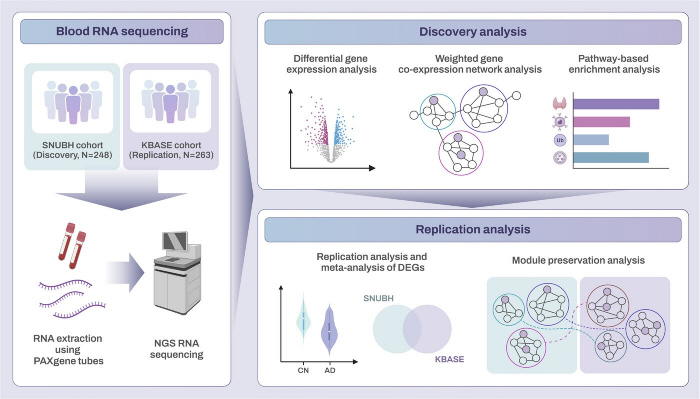
To lower these diagnostic barriers, the research team conducted a study to determine the possibility of early detection of Alzheimer's disease with a simple blood test. The study was conducted by collecting blood samples from 523 Alzheimer's disease patients registered at Seoul National University Bundang Hospital and Seoul National University Hospital and analyzing gene expression patterns through RNA sequencing.
As a result, it was found that 18 genes were expressed in early-onset patients before age 65 and 88 genes in late-onset patients after age 65 in a different pattern than in normal people. In particular, the activity of genes called SMOX and PLVAP was greatly reduced in patients with late-onset Alzheimer's disease, and these genes were found to be closely related to beta-amyloid protein deposition, a major cause of Alzheimer's disease.
The research team also confirmed that genes related to ▲brain cell energy regulation (AMPK signaling pathway) ▲ damaged protein removal (ubiquitin-mediated protein degradation) ▲ intracellular cleaning (mitophage) tend to not work properly in the late-onset group. This is an important biological clue to help us understand more precisely the pathologic mechanisms of Alzheimer's disease.
These results suggest that it shows different gene expression characteristics depending on early/late onset of Alzheimer's disease, and are expected to be an important clue for early diagnosis and development of customized treatment strategies in that they have found clues to distinguish the characteristics of Alzheimer's patients through gene expression information in the blood.
This study is of great academic significance in that it is the first study to systematically compare gene expression in early and late-onset groups in Korean Alzheimer's patients, and is expected to contribute to the development of biomarkers and diagnostic technology specialized for East Asian populations.
Professor Park Young-ho said, "This study is meaningful in that it identifies biological pathways related to the progression of Alzheimer's disease through blood-based gene expression information, and suggests the possibility of early diagnosis and treatment target discovery. We plan to verify the practical clinical applicability through further research on large-scale patient groups in the future."
Meanwhile, the results of this study were recently published in the official journal of the Alzheimer's Disease Association, 'Alzheimer's & Dementia'.
Reporter Jang Jong-ho bellho@sportschosun.com
|
This article was translated by Naver AI translator.