Amyloride Treatment Effect in Resistant Hypertension Patients...Prove the possibility of a fourth antihypertensive drug
May 20, 2025
|
A research team led by professors Park Sung-ha and Lee Chan-joo of Yonsei University Severance Hospital's cardiology department, Shin Dong-ho of integrated medicine, Kim Dae-hee of Asan Hospital's cardiology department, Lim Sang-hyun of circulatory medicine at Bucheon St. Mary's Hospital, and Shin Jin-ho of Hanyang University Hospital's cardiology department announced on the 20th that they confirmed the treatment effect of amyloride as the fourth antihypertensive agent in resistant hypertension patients and that it is not inferior in blood pressure reduction and target blood pressure reach rate compared to the existing treatment, spironolactone.
The results of the study were published in the latest issue of the international academic journal 'JAMA IF 63.1.'
Hypertension, in which more than 30% of adults in Korea suffer, is the most important risk factor for cardiovascular disease. Blood pressure control is essential for the prevention of cardiovascular disease. However, there are many patients with resistant hypertension who cannot control blood pressure even if they take more than three antihypertensive drugs, including diuretics. They have a 1.5 to 2 times higher risk of cardiovascular disease than general hypertensive patients.
In patients with resistant hypertension, additional antihypertensive drugs are taken to control blood pressure. Current guidelines for hypertension recommend adding a potassium-preserving diuretic called 'spironolactone' for patients who take three antihypertensive drugs but cannot control their blood pressure. However, spironolactone is difficult to use because of the risk of side effects such as worsening renal function, amenorrhea caused by sex hormone disturbance, and female-type breast disease.
The research team conducted a randomized clinical study to confirm the effect of reducing pressure of 'Amyloride', which is known to have fewer side effects than spironolactone, although it is one of the potassium-preserving diuretics diagnosed with resistant hypertension at 14 senior hospitals in Korea.
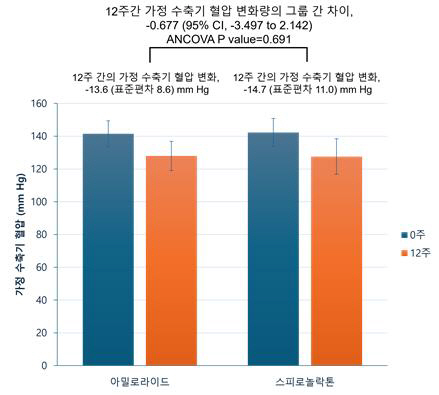
Of 118 patients, 58 were assigned to the amylolide treatment group and 60 to the spironolactone treatment group, and after a total of 12 weeks of medication, the average home systolic blood pressure and the rate of achievement of the clinic's target blood pressure were measured. There were no feature differences between the amyloid group and the spironolactone group at the time of enrollment. At that time, the average home systolic blood pressure in the amyloid group was 141.5 mmHg, and the spironolactone group was 142.3 mmHg.
Analysis showed that the average home systolic blood pressure at 12 weeks compared to enrollment decreased by 14.7 mmHg in the amyloid group and 13.6 mmHg in the spironolactone group. The difference in blood pressure reduction between the two groups was -0.68 mmHg, and there was no statistically significant difference, confirming non-inferiority. The change in home blood pressure at 12 weeks was also well controlled in both groups, both systolic and diastolic blood pressure, and the difference in blood pressure change between the two groups was not significant.
In addition, the home systolic blood pressure 130 mmHg achievement rate was 66.1% in the amyloid group and 55.2% in the spironolactone group, and the office systolic blood pressure 130 mmHg achievement rate was 57.1% in the amyloid group and 60.3% in the spironolactone group, showing no significant statistical difference between the two groups in each area. In particular, there was no difference in the occurrence of drug side effects.
Professor Park Sung-ha "This study confirmed that amyloride has no difference in systolic blood pressure reduction and target blood pressure achievement rate compared to spironolactone in patients with resistant hypertension."It is expected that treatment options for blood pressure control will be added to patients who have had difficulty using the fourth antihypertensive drug due to side effects, etc."
|
This article was translated by Naver AI translator.