New liver cancer immuno-cancer drug combination treatment effectiveness demonstrated...Improvement of survival and objective response rates
May 19, 2025
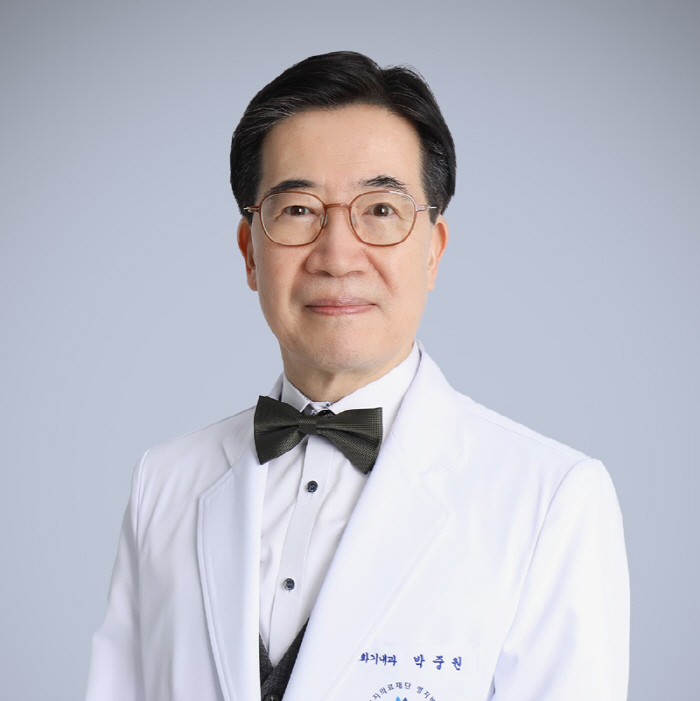
Professor Park Joong-won of the Department of Gastroenterology at Myongji Hospital announced that the combination treatment of new immuno-cancer drugs in HCC can improve survival and tumor reduction effects compared to existing treatments.
This study proved that immune anticancer drug combination therapy can be a better treatment alternative for patients with inoperable hepatocellular carcinoma, which had limitations only with existing drug treatment, and is evaluated as a new turning point in the treatment of hepatocellular carcinoma.
This information was published in the May issue of The Lancet (IF 98.4), a global medical journal, under the title of 'Nivolumab plus ipilimumab verus lenvatinib or sorafenib as first-line treatment for unreserved hepatocellular carcinoma (CheckMate 9DW)'.
'CheckMate 9DW' is a multinational phase 3 clinical trial of 668 inoperable hepatocellular carcinoma patients in 163 hospitals in 25 countries. The research team divided the target patients into two groups, administered immuno-oncology drugs nivolumab and ipilimumab in one group, and administered renvatinib or sorafenib, the existing standard treatment, to the other group to compare and analyze the treatment effect.
As a result, the average survival time of the patient group given nivolumab-ifilimumab immuno-oncology drug was 23.7 months, which was statistically significantly longer than the 20.6 months of the conventional treatment group. The survival rate two years after the start of treatment was 49% in the immune cancer group and 39% in the existing treatment group, and the survival rate after three years was 38% and 24%, respectively, in the immune cancer group.
The objective response rate indicating a decrease in tumor size with treatment was 36% in the immuno-cancer group, nearly three times higher than 13% in the conventional treatment group. The response duration was also 30.4 months on average in the immune cancer group, which was longer than 12.9 months in the existing treatment group.
In addition, 47% of patients who received immuno-cancer drugs continued to respond for 36 months even after the end of treatment, and the incidence of side effects was reported similarly in the two treatment groups, showing relatively good safety.
Professor Park Joong-won said, `This study proved that the new immune cancer combination therapy can be an effective strategy for patients with advanced liver cancer who have difficulty in surgery or other local treatments in extending their survival and reducing cancer""New immuno-oncology combination therapy will improve the patient's choice and effectiveness of treatment along with existing immuno-oncology treatments, thereby increasing survival and improving quality of life.""
Meanwhile, Professor Park is the director of the Liver and Liver Cancer Center at Myongji Hospital and the director of the Cancer Integrated Healing Center, and is leading the development of liver cancer treatment by enacting Korea's first multidisciplinary liver cancer treatment guidelines and investigating the effects of radiation treatment in the world's first liver cancer.
This study proved that immune anticancer drug combination therapy can be a better treatment alternative for patients with inoperable hepatocellular carcinoma, which had limitations only with existing drug treatment, and is evaluated as a new turning point in the treatment of hepatocellular carcinoma.
This information was published in the May issue of The Lancet (IF 98.4), a global medical journal, under the title of 'Nivolumab plus ipilimumab verus lenvatinib or sorafenib as first-line treatment for unreserved hepatocellular carcinoma (CheckMate 9DW)'.
'CheckMate 9DW' is a multinational phase 3 clinical trial of 668 inoperable hepatocellular carcinoma patients in 163 hospitals in 25 countries. The research team divided the target patients into two groups, administered immuno-oncology drugs nivolumab and ipilimumab in one group, and administered renvatinib or sorafenib, the existing standard treatment, to the other group to compare and analyze the treatment effect.
As a result, the average survival time of the patient group given nivolumab-ifilimumab immuno-oncology drug was 23.7 months, which was statistically significantly longer than the 20.6 months of the conventional treatment group. The survival rate two years after the start of treatment was 49% in the immune cancer group and 39% in the existing treatment group, and the survival rate after three years was 38% and 24%, respectively, in the immune cancer group.
The objective response rate indicating a decrease in tumor size with treatment was 36% in the immuno-cancer group, nearly three times higher than 13% in the conventional treatment group. The response duration was also 30.4 months on average in the immune cancer group, which was longer than 12.9 months in the existing treatment group.
In addition, 47% of patients who received immuno-cancer drugs continued to respond for 36 months even after the end of treatment, and the incidence of side effects was reported similarly in the two treatment groups, showing relatively good safety.
Professor Park Joong-won said, `This study proved that the new immune cancer combination therapy can be an effective strategy for patients with advanced liver cancer who have difficulty in surgery or other local treatments in extending their survival and reducing cancer""New immuno-oncology combination therapy will improve the patient's choice and effectiveness of treatment along with existing immuno-oncology treatments, thereby increasing survival and improving quality of life.""
Meanwhile, Professor Park is the director of the Liver and Liver Cancer Center at Myongji Hospital and the director of the Cancer Integrated Healing Center, and is leading the development of liver cancer treatment by enacting Korea's first multidisciplinary liver cancer treatment guidelines and investigating the effects of radiation treatment in the world's first liver cancer.
|
This article was translated by Naver AI translator.