Successful Artificial Joint Surgery of a Preserved Knee Robot The First Identification of Left and Right Tibial Rear Sections
May 20, 2025
|
With the entry of an ultra-aging society, knee artificial joint surgery due to degenerative arthritis is increasing. According to statistics from the Health Insurance Review and Assessment Service, the number of artificial joint surgery cases in 2024 is about 120,000 cases, which is steadily increasing every year and has increased by about 7.5% in three years.
Recently, as the use of robots in artificial joint surgery has expanded, research on precise robot artificial joint surgery techniques is also being actively conducted. This is to improve the prognosis of patients by using robots to increase surgical accuracy.
In conventional artificial joint surgery, it was common to remove the posterior cruciate ligament and make the patient's legs straight after the surgery. This method had the advantage of reducing the burden on artificial joints, but patients felt heterogeneous and uncomfortable in changing the patient's unique knee movement and adapting soft tissues such as tendons and muscles formed to fit the leg structure and shape to the new leg shape. To improve this problem, Professor Kim Joong-il's team studied a surgical method that preserves the posterior cruciate ligament and finds the optimal leg shape for each patient 'Patient-customized Preserved Robot Artificial Joint Surgery'.
The tibia posterior oblique angle is an angle indicating how much the joint surface is tilted backward when viewed from the side of the lower knee bone (tibia), showing unique differences for each individual. This angle has an important effect on the function of the posterior cruciate ligament, as well as the stability of the knee and the kinematics of the joint.
In particular, during conservative artificial joint surgery, if the tibia posterior oblique angle is not accurately reproduced, the natural flexion of the knee becomes difficult, and postoperative pain, stiffness, and flat or stair walking can be deteriorated. In this regard, in conservative artificial joint surgery, it is very important to accurately reproduce the posterior tibia oblique angle in consideration of the shape of the tibia before surgery.
|
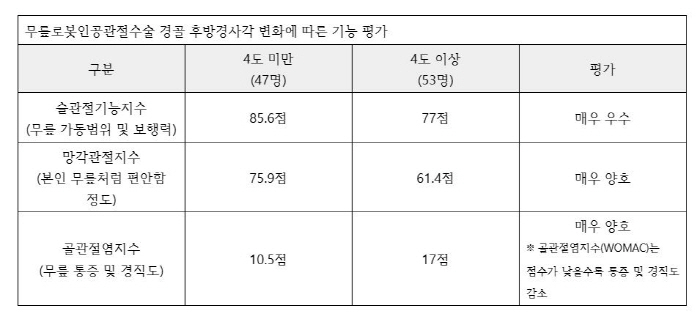
The research team analyzed the prognosis of patients based on the △Knee Society Function Score △ Forgotten Joint Score △ Osteoarthritis Index (WOMAC).
As a result, significant differences were observed in the group that maintained the patient-specific posterior tibia oblique change less than 4 degrees and the group that changed more than 4 degrees. Even after surgery, the patient's unique posterior tibial oblique was reproduced in the group, which felt more comfortable like one's own knee when walking up and down the stairs. This is analyzed as a result of accurately reflecting the patient's unique anatomical characteristics using robots.
Professor Kim Joong-il said, "The results of this study demonstrate that identifying the patient's unique posterior tibia oblique angle before surgery and reflecting it in surgery greatly helps improve the prognosis. "We believe that it will contribute to the rapid recovery and improvement of walking satisfaction of patients who were not satisfied with existing artificial joint surgery." "
Professor Kim then added, "The recent topic of artificial joint surgery lies in 'personalization'," adding that "True treatment is not to perform surgery in the same way for all patients, but to precisely analyze the anatomical structure of each patient and implement the most appropriate alignment for the patient."
The results of this study were recently published in the official journal of the European Sports Medical Association 'KSSTA (Knee Surgery Sports Traumatology Arthroscopy)'.
|
This article was translated by Naver AI translator.