Bladder cancer recurrence, urine acidity predictable...Expectation of Customized Treatment
|
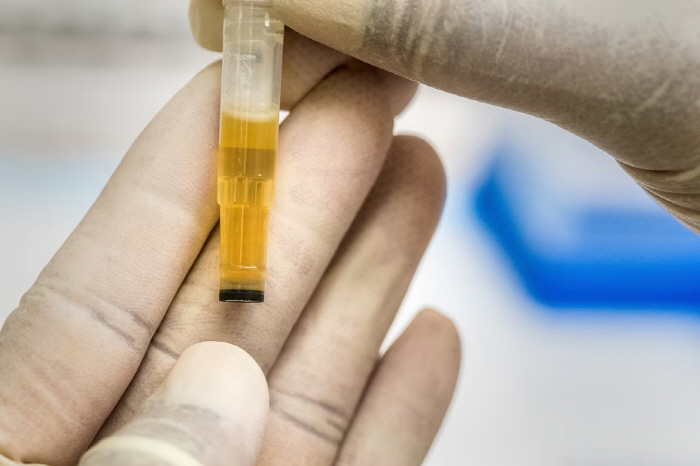
Non-muscle invasive bladder cancer is a relatively early stage cancer that has not spread to the muscle layer of the bladder wall, accounting for about 70% of all bladder cancer patients. Although the tumor can be removed by surgery, the risk of recurrence is high, so adjuvant treatment is performed by injecting BCG (a tuberculosis-derived immunotherapy) into the bladder after surgery. However, bladder cancer is known to recur in about 40% of patients even after BCG treatment, raising the need to develop indicators that can predict the treatment response in advance.
According to previous studies, it is known that an acidic environment can reduce the effectiveness of immunotherapy by inhibiting the activity of immune cells.
Therefore, the research team wanted to determine how acidity in the bladder actually affects the treatment effect, assuming that BCG treatment based on immune response can also be affected by this acidic environment.
The research team analyzed data from 578 patients with non-muscle invasive bladder cancer who received BCG treatment after bladder cancer resection from 2003 to 2021. The recurrence rate of bladder cancer was compared by dividing the urine before treatment into 'acid urine group' and the case of abnormalities into 'acid urine group'.
As a result, the recurrence rate of the acid urine group was found to be 42.4% and the non-acid urine group to be 33.8%, showing a significant difference in the recurrence rate after BCG treatment. In addition, in a multivariate analysis that considered other recurrence risk factors such as age, smoking history, size and number of tumors, acid urine was found to be an independent risk factor that increased the risk of bladder cancer recurrence by about 45%.
This study is significant in that it identified that urine acidity can affect BCG treatment response and suggested the possibility of using it as a prognostic indicator. Based on this, it is expected that simple urine tests before treatment will predict the patient's treatment response and contribute to establishing personalized treatment strategies in the future.
Professor Lee Sang-chul of the Department of Urology at Seoul National University Bundang Hospital said, `Non-muscle invasive bladder cancer is a disease that often causes a heavy burden on patients as cancer recurs or treatment effects are limited even after treatment.' `This study suggests the possibility of predicting treatment responses even with non-invasive methods such as urine tests, which can help establish effective treatment strategies while reducing the burden on patients in the future.'
Then, Professor Song Byung-do of the Department of Urology at Hanyang University's Guri Hospital said, "Based on the results of this study, we plan to review whether BCG treatment response can be improved by controlling acidity in the bladder, and continue research to establish a clinical basis to prove this."
Meanwhile, the results of this study were published in the SCIE-level international journal 'World Journal of Urology'.
|
This article was translated by Naver AI translator.