What is a lifeline arteriovenous fistula composition in hemodialysis patients?
|
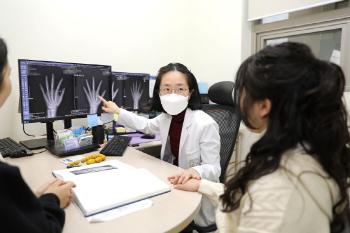
Professor Choi Earl of Vascular Surgery at Soonchunhyang University Bucheon Hospital said, `Because hemodialysis is difficult with common veins, a dialysis blood vessel called 'bronchial fistula' should be made with thick and high blood flow. He explained that the surgery for this is arteriovenous fistula composition.
An arteriovenous fistula is literally a method of connecting arteries and veins to secure a passage with abundant blood flow. Initially, dialysis can be started temporarily through the insertion of 'Jugular Catheter', but long-term use is difficult due to the high risk of infection. Therefore, most patients undergo arteriovenous fistula surgery to stably maintain dialysis. Although arteriovenous fistula composition is generally possible for both arms or legs, it is usually considered from the arm in consideration of complications and lifespan.
In surgery, an appropriate blood vessel is first selected through ultrasound, and then the skin is incised under partial anesthesia to connect arteries and veins. The method is divided into 'autologous vascular arteriovenous fistula' that connects the patient's blood vessels directly and 'artificial vascular arteriovenous fistula' that connects the arteriovenous veins using artificial blood vessels.
Autologous vascular arteriovenous fistula has a low risk of infection, but requires 6-8 weeks for vascular maturation, and artificial blood vessels can be used relatively quickly after about 4 weeks, but the risk of infection and vascular occlusion is greater than that of autologous blood vessels. If the existing blood vessel condition is not good enough, the blood vessel is not thick enough, which may require reoperation or additional procedures to help blood vessel maturation.
An arteriovenous fistula surgery is generally possible to be discharged on the day of surgery if there are no acute complications. Above all, postoperative care is important. Autologous vascular arteriovenous fistula requires sufficiently thick and hard blood vessels to poke dialysis needles, so it is recommended to repeat the exercise of lightly holding and opening hands or holding and opening rubber balls at least five times a day.
In addition, blood pressure measurement, blood collection, and intravenous injection should be avoided on the arm at the surgical site, and arm arms, arm pillows, heavy lifting, tight sleeves or bracelets should be avoided. Blood vessel damage can lead to excessive bleeding, so special care is needed.
A normal arteriovenous fistula feels a 'winging' vibration when touched by hand. If the vibration disappears, or the arm is swollen and painful, you should visit the hospital immediately. This can be an abnormal signal such as vascular stenosis, obstruction, or infection.
An arteriovenous fistula can cause complications of narrowing or clogging when used for a long time. In this case, the problem may be solved through percutaneous angioplasty or thrombectomy, or an arteriovenous fistula may be newly created if necessary.
Professor Choier emphasized that "the sinus venous fistula is not just a blood vessel, but a lifeline for patients with end-stage renal failure" and that "thorough management after surgery is the key to successful dialysis treatment."
|
This article was translated by Naver AI translator.