Liver cancer immune cancer treatment effect, predicted by a drop of blood...Development of a New Biomarker PBIS
Sep 23, 2025
|
Liver cancer, which ranks third in terms of cancer death worldwide, is also improving its treatment performance due to the development of various treatments. Recently, immune anticancer combination therapy has been applied as the first standard treatment for inoperable advanced liver cancer, increasing the survival rate, but about 30% of patients are effective, and it is urgent to select a patient group that will respond well to the treatment and establish a customized treatment strategy for each patient.
Meanwhile, a research team led by Han Ji-won (corresponding author) and Cho Hee-sun (co-author) of the Department of Gastroenterology at Seoul St. Mary's Hospital, and Lee Soon-kyu (co-author) of the Department of Gastroenterology at Incheon St. Mary's Hospital have developed a blood index that can predict the treatment response of atezolizumab-bevacizumab (AB) combination therapy, which is widely used as the first-line treatment for advanced liver cancer patients.
To verify predictive power, the research team conducted the first multicenter prospective study in Korea on advanced liver cancer patients receiving the treatment from May 2020. A total of 170 patients were analyzed, 116 patients who received immuno-cancer treatment at Seoul St. Mary's Hospital and 54 patients treated at Incheon St. Mary's Hospital outside of Seoul to verify their predictive power.
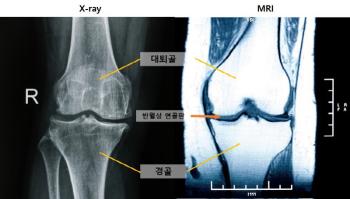
PBIS mainly consists of evaluation indicators in different meanings that evaluate the activity of cancer-fighting immune cells and their adherence to immune responses. The evaluation indicators were neutrophil-lymphocyte ratio, C-reactive protein, interleukin-2, and interleukin-12, which were classified as 'risk groups' if more than two of them were above the normal threshold.
As a result, the group with high PBIS levels had significantly poor prognosis of overall survival, progression-free survival without disease progression, and objective response rate of treatment.
To demonstrate the accuracy of the prediction method, the statistical analysis of 'propensity score matching' showed that the risk of death was 3.6 times higher and the risk of progression was 2.1 times higher in the group with high PBIS levels.
On the other hand, in the renbatinib treatment group, the first-line targeted treatment for liver cancer, PBIS failed to predict the treatment response, suggesting that PBIS is a biomarker, especially effective only in the combination of atezolizumab-bevacizumab.
Liver cancer treatment is divided into radical treatments such as surgery, liver aches, and high-frequency heat therapy, and conservative treatments such as hepatic artery chemoembolization, targeted anticancer therapy, and radiation therapy. Progressive liver cancer, which refers to a state of advanced stage due to vascular infiltration or metastasis among liver cancer, is also improving its survival with the recent development of various treatments including immuno-oncology drugs. The application of health insurance also reduced the cost of treatment for patients, but it did not show the same effect on all patients, so a biomarker was needed to predict patient treatment responses and select patients.
Professor Han Ji-won of Seoul St. Mary's Hospital said, "This study is meaningful in that it has presented the possibility of predicting the immune cancer treatment response through non-invasive blood indicators in patients with advanced liver cancer. PBIS will contribute to the establishment of optimal treatment strategies by reflecting the individual patient's inflammatory status and immune response."
Professor Cho Hee-sun of Seoul St. Mary's Hospital explained that `Interleukin-2 and Interleukin-12 are factors involved in both immune activity and inhibition, and this study has improved prediction accuracy by integrating these cytokines and traditional inflammatory indicators.'
Professor Lee Soon-kyu of Incheon St. Mary's Hospital said, "The effectiveness of immune cancer treatment in patients with advanced liver cancer is often limited, so it is urgent to develop a biomarker for patient selection. This study verified the clinical usefulness of PBIS through multicenter prospective studies, and is expected to lead to more precise customized treatment in the future."
The results of the study, supported by the Ministry of Health and Welfare and carried out through the Korea Health Industry Promotion Agency, were recently published in the international academic journal Frontiers in Immunology.
|
This article was translated by Naver AI translator.