Physician-based medical care demonstrates effectiveness in reducing medical costs for diabetics
Oct 24, 2025
|
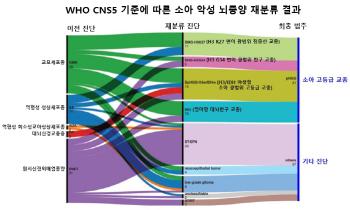
The term "usual source of care" (USC) refers to a doctor or medical institution that regularly visits a patient when he or she is sick or needs health counseling. The research team classified the types of commercial treatment centers for diabetic patients into 'if there is no designated doctor and medical institution at all', 'if only medical institution is designated', and 'if both doctors and medical institutions are designated'. In particular, 'when both doctors and medical institutions are designated' was divided into high quality and low quality according to the inclusiveness and coordination of the treatment evaluated by the patient.
The research team analyzed data from 6,144 patients with diabetes on the Korean Medical Panel from 2019 to 2022.
Korea has the highest hospitalization rate due to diabetes among OECD member countries, and diabetes management is still poor enough that the number of years of disability-corrected survival due to diabetes among high-income countries in 2021 reached a record high of 966.4 per 100,000 people. Diabetes is an effective outpatient treatment that can reduce hospitalization and emergency room visits, and the prognosis of treatment may vary through systematic management in local medical institutions.
During the study period, the proportion of diabetic patients with both doctors and medical institutions increased by 7.6% from 58.5% in 2019 to 66.1% in 2022, and the number of patients without doctors and medical institutions decreased by 4.2% from 15.1% to 10.9%. In the early days of COVID-19 in 2020, the number of temporary breakups in the family doctor relationship among the vulnerable increased, but in 2022, it recovered and showed an overall improvement trend.
Patients with commercial treatment centers during COVID-19 were found to have effectively suppressed the rise in medical expenses compared to those who did not. Patients without both doctors and medical institutions saw their medical expenses soar 55.4%, while patients with only medical institutions rose 35.6%, but patients with both doctors and medical institutions increased only 3.6%. This shows that continuous management through a dedicated doctor, a doctor, effectively suppressed the rise in medical expenses even in crisis situations.
In addition, as a result of a precise analysis of patient characteristics and disease severity, it was confirmed that among patients who have been consistently treated by both doctors and medical institutions, patients with high-quality doctors showed 13.1% lower medical expenses than patients without both doctors and medical institutions. This shows that establishing a continuous relationship with a specific doctor and receiving comprehensive medical treatment are more effective in reducing medical expenses than simply setting up a medical institution you usually attend.
In particular, during the study period, the COVID-19 period was a period when the problems of chronic disease management were revealed significantly, and diabetic patients suffered greatly due to hospital closure and decreased access to treatment. However, it is evaluated that this helped prevent the rise in medical expenses, as patients with family doctors were able to receive appropriate drugs on time and check their blood sugar through telemedicine and electronic prescriptions. This is consistent with international studies showing that if diabetics maintain an ongoing relationship with their physician, they improve drug compliance, use many preventive services, reduce complications, and lower overall medical costs.
Professor Lee Jae-ho explained, `This study provides a policy basis for diabetics with the right doctor to not only reduce treatment progress but also effectively lower medical costs.'
Professor Shin Hyun-young said, `If the pilot project of the family doctor promoted by the new government can be designed as a comprehensive health care program that satisfies both doctors and patients by reflecting the medical reality of Korea, meaningful results for health aging in the super-aging era can be achieved.'
The study was published in the October issue of the international journal BMC Health Services Research.
|
This article was translated by Naver AI translator.