Seoul National University Hospital reclassifies the WHO standard for childhood malignant brain tumors...Determination of prognosis and genetic characteristics
Oct 24, 2025
|
Childhood malignant brain tumors account for about 20% of all childhood cancers and are one of the leading causes of childhood cancer death. Among them, pediatric high-grade glioma is a malignant tumor that occurs in glial cells in the brain, and is an incurable disease with rapid growth, frequent recurrence, and poor prognosis despite treatment. Recent studies have confirmed that these pediatric high-grade gliomas are an independent biological and genetic disease group that is completely different from glioblastomas that occur in adults, raising limitations in how diagnosis and treatment have been applied based on existing adult standards.
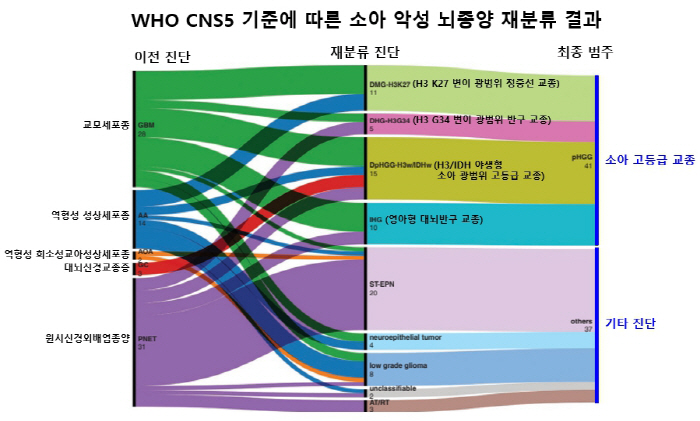
Accordingly, the 5th edition of the WHO Central Nervous System Tumor Classification (WHO CNS5) revised in 2021 removed the diagnostic names of previous pediatric glioblastomas and primary neuroextraembolic tumors and introduced a new category of 'pediatric-type broad-type diffuse high-grade glioma'. This category is divided into four molecular subtypes: the H3 K27 variant, the H3 G34 variant, the H3/IDH wild type, and the infant type.
The research team of professors Kim Seung-ki and Kim Joo-hwan of pediatric neurosurgery at Seoul National University Hospital and Park Sung-hye of the Department of Pathology conducted a pathological review of 78 tissues diagnosed with glioblastoma, anaplastic astrocytoma, anaplastic glioblastoma, cerebral glioblastoma, and primitive neuroextraembolic tumors from 1997 to 2023 and conducted immunochemical staining and next-generation nucleotide sequence analysis (NGS) targeting brain tumors to perform integrated diagnosis according to WHO CNS5 standards.
As a result, 41 (52.6%) of the 78 total were reclassified to 'Children's High Level Glioma (pHGG)'. The detailed subtypes were ▲H3K27 mutant wide midline glioma (DMG-H3K27) 11 ▲H3G34 mutant wide hemispheric glioma (DHG-H3G34) 5 ▲H3/IDH wild-type pediatric wide-level high-level glioma (DpHG-H3wt/IDHwt) 15 ▲Young-type cerebral hemispheric glioma (IHG). This result shows that it was difficult to clearly distinguish the prognosis for each disease with the existing diagnostic system, and that the integrated classification with the latest WHO criteria can increase clinical predictive power.
The research team then applied the WHO CNS5 criteria to reclassified patients and added 20 newly diagnosed pHGGs to compare and analyze a total of 61 clinical and genomic information. Among them, TP53 gene mutations were identified in 34 (70.8%) of 48 people who were able to analyze the genome except for infant-type cerebral hemisphere gliomas.
In particular, the H3/IDH wild-type pediatric wide-level glioma subtype was accompanied by cancer-causing syndrome such as Li-Fraumeni syndrome, neurofibromatosis type 1 (NF-1), and genetic mismatch recovery deficiency syndrome (cMMRD), suggesting that germ cell genetic analysis and family counseling are essential when diagnosing high-level gliomas in children.
As a result of prognostic analysis, infant-type cerebral hemispheric glioma had a statistically significant survival rate compared to other subtypes (p<0.0001). The 2-year survival rate was 92.3% and the 5-year survival rate was 73.8%, and the patient group who underwent preoperative resection (GTR) had a significantly higher survival rate than the non-GTR patient group (p<0.0001). The research team explained that considering the characteristics of infant development and the relatively good prognosis, unnecessary radiation therapy can lead to long-term side effects, requiring a customized approach to adjust the intensity of treatment according to patient condition and scope of surgery.
Professor Kim Seung-ki (Pediatric Neurosurgery) said, "This study is a meaningful study that re-analyzed patients diagnosed with childhood glioblastoma in the past in molecular pathology and identified the exact classification and prognosis of pediatric high-grade glioblastoma. We look forward to contributing to the establishment of patient-specific treatment strategies and improvement of prognosis in the future."
The study was carried out with the support of Lee Kun-hee's Childhood Cancer and Rare Disease Support Project Group, and was recently published in the international academic journal 「Neuro-Oncology Advances」.
|
This article was translated by Naver AI translator.