One in five pregnant women over the age of 35 have gestational diabetes...When is the examination?
Mar 16, 2025
|
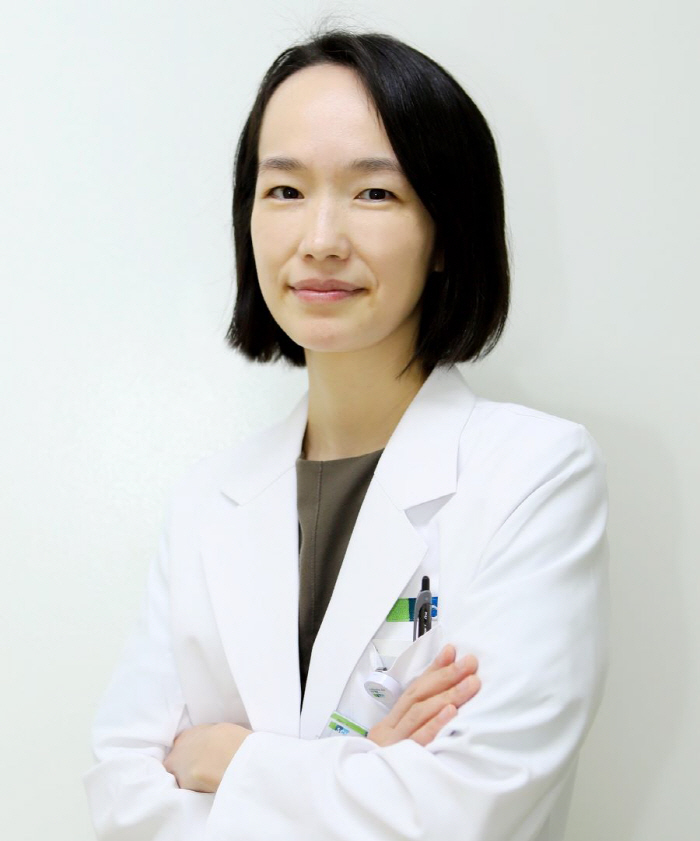
With the help of Professor Cho Yoon-young of the Department of Endocrine Metabolism at Soonchunhyang University Bucheon Hospital, we summarized gestational diabetes.
◇19.4% prevalence of gestational diabetes in pregnant women over 35 years of age
During pregnancy, fasting blood sugar is lowered because sugar is consumed in the fetus and placenta, but carbohydrate intolerance tends to increase blood sugar after meals. In the early stages of pregnancy, insulin sensitivity increases and blood sugar decreases, but in the second and third trimesters of pregnancy, insulin resistance increases and blood sugar may rise. Pregnant women with normal pancreatic function can compensate for these changes, but if insulin resistance is not overcome, blood sugar rises abnormally, which is called 'pregnant diabetes'. This condition improves rapidly as the placenta is discharged after childbirth.
The prevalence of gestational diabetes is on the rise worldwide. The domestic prevalence rate continued to increase every year from 4.1% in 2007 to 12.7% from 2011 to 2015. Major risk factors for gestational diabetes include ▲aged pregnancy (35 years of age or older) ▲ obesity (BMI of 25 or more, waist circumference of 85 cm or more) ▲ high fasting blood sugar ▲ family history of type 2 diabetes. The prevalence tends to increase with age and higher BMI. The prevalence of gestational diabetes in pregnant women over 35 years of age
Gestational diabetes is mostly asymptomatic, so screening is important. If you have a history of gestational diabetes in the past, have a family history of type 2 diabetes in your immediate family, have had a giant baby birth of more than 4kg, or have an fasting blood sugar rise, you may be screened at 18 weeks.
◇It is irrelevant to the occurrence of deformity, but it can cause the delivery of giant babies and hypoglycemia in newborns
Pregnant diabetes occurs after the middle of pregnancy, so it is not related to the occurrence of malformations. However, high blood sugar in pregnant women can promote excessive growth of the fetus, causing giant babies weighing more than 4 kg (22% or more), or neonatal hypoglycemia (13% or more) due to excessive insulin secretion in the fetus immediately after delivery. In addition, the risk of complications such as neonatal jaundice (15% or more), dyspnea (5% or more), and erythema (3% or more) also increases. In addition, in the long run, there is a possibility that children will be obese from the time of elementary school, or that they will develop into glucose tolerance, which increases fasting blood sugar from adolescence to the age of 14-16.
All pregnant women are screened for gestational diabetes between 24 and 28 weeks. There is a possibility of gestational diabetes if blood sugar glucose is measured an hour after 50g glucose intake without a separate preparation and 140mg/dL or more. At this time, an additional 100g oral load test is performed for more accurate diagnosis. The oral sugar load test checks blood sugar after fasting for more than 8 hours before the test while eating an appropriate amount of meals on time and evenly 3 days before the test. Blood sugar standards are based on 105mg/dL on an empty stomach, 190mg/dL after 1 hour, 165mg/dL after 2 hours, and 145mg/dL after 3 hours, and if more than two criteria are exceeded, it is diagnosed as gestational diabetes. If only one out of four blood glucose is high, a re-examination can be performed between 32 and 34 weeks.
Treatment goals for gestational diabetes are maintenance of normal blood sugar, proper weight gain, and prevention of ketoacidosis. The normal blood sugar target is ▲ less than 95mg/dL of fasting blood sugar ▲ less than 140mg/dL of blood sugar for 1 hour after meals ▲ less than 120mg/dL of blood sugar for 2 hours after meals. Although blood sugar can be controlled mostly by diet and exercise, about 10-15% of pregnant women may need insulin injection treatment. Ketone is a decomposition product that comes out when fat is used as an energy source, and is a danger signal identified in blood sugar or urine when glucose is not sufficiently used as an energy source. Ketonic acidosis can occur when a meal is not consumed sufficiently, meals and snacks are delayed for too long, or when insulin in the body is insufficient.
◇More than half of women with gestational diabetes are at risk of developing diabetes for life
Pregnant weight should be increased slowly. Weight gain of 1 to 2 kg in the early pregnancy (last menstrual start date to 13 weeks) and 0.2 to 0.5 kg per week from the second trimester (14 to 28 weeks) are appropriate. Daily food intake and exercise are recorded for proper weight gain, and counseling is required during treatment or education when there is a weight change that is different from normal.
Diet therapy for gestational diabetic patients basically consists of three even meals and two to three snacks. Grain is better than rice, fresh fruits and vegetables are better than juice. Eating vegetables, seaweed, mushrooms and high-quality protein is recommended for every meal. To prevent hypoglycemia and ketoemia overnight, it is good to eat snacks such as milk and small amounts of fruit before bed. However, simple sugars such as honey, candy, chocolate, snacks, and ice cream that cause a sudden rise in blood sugar should be avoided.
Exercise during pregnancy improves insulin resistance, facilitates blood sugar control, and prevents obesity. It is recommended to break the news 30 minutes after eating, for 20-30 minutes, five times a week. Fixed bicycles or upper body exercises with less weight are also good. However, if you have had a miscarriage more than three times or have a risk of premature birth, or if you have multiple pregnancy or gestational hypertension, you must consult with a medical staff.
Professor Cho Yoon-young said "If pregnancy diabetes is detected early and actively managed, healthy childbirth is possible. However, women who have experienced gestational diabetes need continuous blood sugar management even after childbirth. 50-60% of women who suffer from gestational diabetes are at risk of developing diabetes for life afterwards, and the risk of developing diabetes steadily increases to 20% after 10 years and 30% after 20 years. Therefore, you should pay constant attention after childbirth, check your blood sugar status through regular checkups, and maintain a healthy lifestyle," he said.
|
This article was translated by Naver AI translator.