Electronic drug direct current stimulation of the transcranial head, and patients with skull damage can also be treated
May 13, 2025
|
Transcranial Direct Current Stimulation (tDCS) treatment, which is used as nerve control treatment, had limitations that patients with skull damage due to trauma and surgery could not use it. The treatment is a method of attaching electrodes to the scalp and dispersing it through the highly current-resistant skull to reach the desired area, but if there is skull damage, the flow of current to the damaged area may change, affecting areas other than the treatment target.
Meanwhile, a research team led by Professor Lim Sung-hoon (co-corresponding author) of Seoul St. Mary's Hospital and Professor Yoon Mi-jung (first author) of St. Vincent's Hospital compared five patients with skull injuries caused by brain surgery and five control groups who had never undergone brain surgery and were aged. It is a joint study with Dr. Kim Dong-hyun (co-corresponding author) of Neuropit, a company specializing in artificial intelligence technology-based brain disease solutions, and Dr. Yasin Y. Dhaher, a professor of biotechnology and rehabilitation medicine at the University of Texas in the United States.
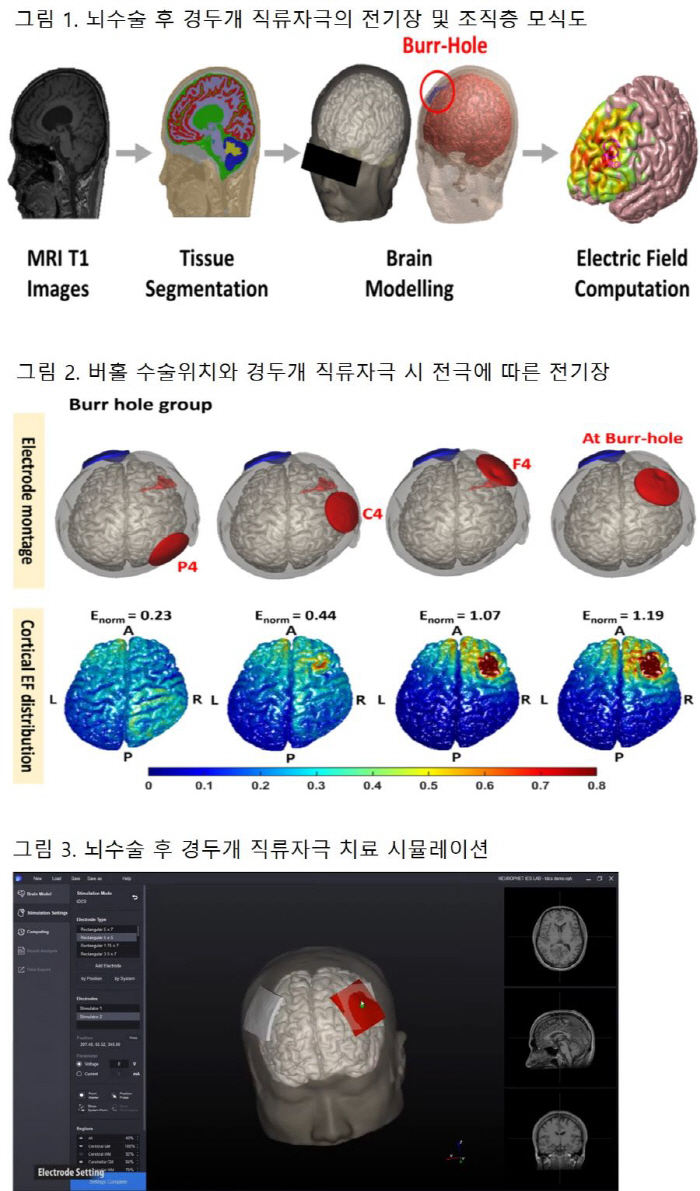
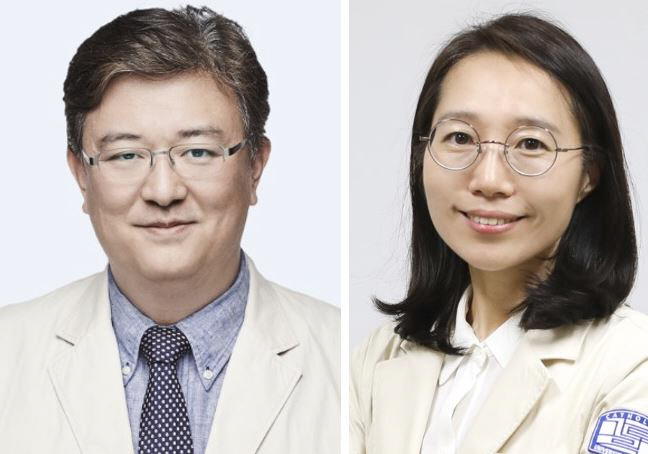
An MRI scan image was analyzed to create a digital brain model, simulate transcranial direct current stimulation treatment in a virtual environment, and analyze the flow of electric fields and currents affecting the brain cortex. The study confirmed that safe and effective electric field strength can be obtained by adjusting the electrode position 60 mm away from the burr hole, a skull hole, to prevent unintended stimulation in the brain cortex during treatment.
Transcranial direct current stimulation is a type of neuromodulation that stimulates nerve cells in the brain by flowing fine direct current through the anode and cathode electrodes attached to the skin surface (cranial). First of all, nerve cell activity near the stimulation site is controlled, but treatment is carried out on the principle of affecting the nerve circuit inside the brain by utilizing the nerve cell characteristics that form interconnected networks. It improves brain function by locally stimulating certain areas of the brain in a pain-free and safe way for patients with brain function damage. Patients with decreased motor or cognitive function after brain diseases such as stroke, traumatic brain injury, and brain tumors are eligible for treatment.
The treatment is non-invasive and is only about 1/1000th of the level of current (up to 2mA) and electromagnetic waves (about 0.001W/kg) exposure compared to smartphones, so there is not much risk to human body and side effects. However, treatment has been considered taboo for patients with damaged skulls, such as Burhole surgery patients who drill holes in the skull to drain blood to remove hematomas caused by cerebral hemorrhage.
Professor Sung-Hoon Lim said "It is known that the scalp dents around the burhole area after surgery, and we actually identified and reflected these structural changes with the patient's MRI imaging."It will be useful data for the development of safe and effective treatment for cranial direct current stimulation treatments for patients with skull injuries in the future."
Professor Lim Sung-hoon's research on neuromodulation therapy using artificial intelligence software was recently published in the prestigious medical information journal Computers in Biology and Medicine, which is part of the Korea Research Foundation's extensive research and was conducted with international collaboration with researchers from the University of Texas at the support of the Basic Medical Project of the Catholic Medical Center.
|
This article was translated by Naver AI translator.