Alzheimer's disease is completely discriminated, and tweezers are found...World's First Proof
Jun 12, 2025
|
Meanwhile, U.S. and Korean researchers conducted an international joint study and reported the world's first method of detecting Alzheimer's pathology using blood.
Professor Cho Han-na of the Department of Neurology at Yonsei University's Gangnam Severance Hospital formed an international joint research team with Professor Lawren VandeVrede of the University of California (UCSF) Memory and Aging Center to observe clinical manifestations of various degenerative brain diseases.
Dementia is divided into several branches according to various causative diseases, starting with Alzheimer's disease, which has typical symptoms, and has different clinical features and pathological mechanisms. It is difficult to distinguish only by clinical symptoms, and there were many limitations on diagnostic tools that could be applied because several causes were mixed. PET scans, cerebrospinal fluid tests, and MRI scans have been used as diagnostic tools, but each has limitations.
In response, the research team recently announced p-tau217 (blood-based biomarker), a biomarker that accurately reflects the key pathological mechanisms of Alzheimer's disease. The research began to examine the usefulness of the substance and the possibility of using it as an alternative to diagnosing next-generation dementia (FTLD) test indicator.
The research team targeted a total of 349 subjects (55% male, 72-year-old average at death) who underwent clinical evaluation at UCSF Memory and Aging Center from August 2008 to July 2022 and donated post-mortem brain tissue. This is the world's highest level in the brain pathology-confirmed cohort and blood data segment.
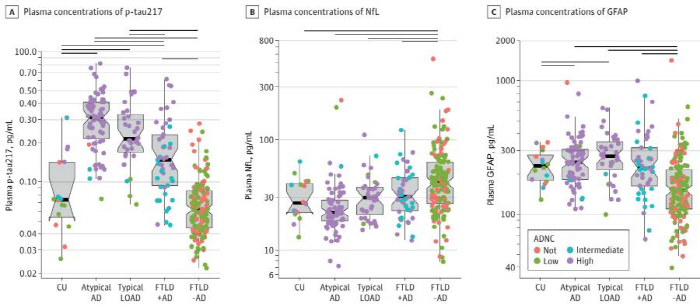
In the study group, patients with various degenerative brain diseases, including Alzheimer's disease patients and normal people for control, were included in the study group. The research team extracted three biomarkers from the blood data: p-tau217 and Neurofilament Light Chain (NfL), which shows the degree of nerve damage, and Glial Fibrillation Acidic Protein (GFAP), which shows the state of nervous system inflammation, and simultaneously observed the concentration with a Precision Analysis Equipment (SIMOA).
As a result of the study, the p-tau217 concentration (average 0.28 pg/mL) of the Alzheimer's disease group was significantly higher than that of the frontal brain dementia patients (average 0.10 pg/mL) in the blood test measured after the death (P<.05). The concentration of p-tau217 (average 0.19 pg/mL) in patients with frontal temporal lobe dementia with Alzheimer's disease was also significantly higher than that of those without Alzheimer's disease (average 0.07 pg/mL).
As a result, it was concluded that the p-tau217 substance in the blood was very good for diagnosing the neuropathology of Alzheimer's disease. In all dementia-related syndromes, the diagnostic accuracy of Alzheimer's disease (AUC) was maintained at 0.95, showing a very high level. In particular, the typical Alzheimer's group showed an accuracy of 0.98 (AUC), and maintained a relatively accurate performance of 0.89 even without the Alzheimer's disease group.
On the other hand, NfL and GFAP, which were highly anticipated as biomarkers, showed low scores in the accuracy of diagnosis of Alzheimer's disease.(AUC 0.73, 0.75 respectively) In addition, it did not significantly increase the diagnostic value when used in combination with p-tau217 substances.
In addition, the research team revealed that about 23% of patients diagnosed with anterior temporal dementia had Alzheimer's pathology together. When two forms of dementia were accompanied, they showed a worse degree of performance across the cognitive domain, including memory, execution function, and space-time ability, including cognitive function test scores (MMSE). In addition, severe cortical atrophy behind the brain was also reported.
Professor Johanna, who played a leading role in this study, said "The research results are very high in that blood-based p-tau217 substances are the first in the world to prove that Alzheimer's pathology can be accurately detected in various dementia patients." In the future, p-tau217 substances are expected to be key tools for accurate differential diagnosis, treatment selection, and prognosis prediction. It is significant because it not only marks a turning point in Korea's dementia diagnosis and research environment entering a super-aged society, but also provides a foothold for the establishment of standards for early diagnosis and treatment of dementia based on blood in the future.
The results of this study were recently published in the world's leading medical journal, 'JAMA Neurology', in the field of neuroscience.
|
This article was translated by Naver AI translator.