I thought it was a cold, but pyelonephritis?If left unattended, it can cause sepsis and renal failure
Sep 09, 2025
|
#. B, a woman in her 40s, thought it was cold and feverish after playing in the water recently. Even after taking cold medicine, the symptoms worsened and I visited the hospital, but the test showed that it was acute pyelonephritis.
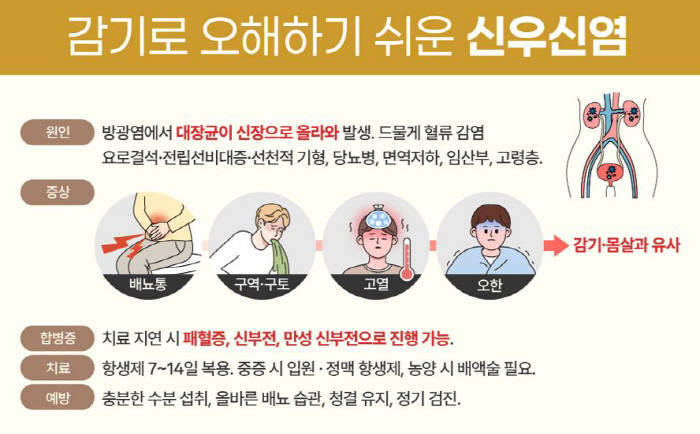
Recently, there is an increasing number of cases in which patients mistake pyelonephritis for a simple cold or body aches and miss the timing of treatment. Pyelonephritis is a serious urinary tract infection disease caused by bacteria penetrating the kidneys, although its initial symptoms are similar to common colds such as fever, chills, and fatigue. Missing the timing of treatment can lead to fatal complications such as sepsis and renal failure.
The most common cause of pyelonephritis is ascending urinary tract infection. More than 80% of all patients are caused by bacteria coming back from cystitis and reaching the kidneys, and most of the causative bacteria are E. coli. Rarely, hematogenous (through blood) infection is also possible. Infections in other areas, such as skin abscesses, endocarditis, and sepsis, can occur as they penetrate the kidneys through the bloodstream.
In addition, bacteria easily proliferate if urine flow is blocked due to urinary structural abnormalities such as urinary stones, congenital malformations, and prostate hypertrophy. The risk of developing pyelonephritis also increases for patients with weakened immune systems, such as diabetics, patients undergoing chemotherapy, and patients taking long-term immunosuppressants.
In terms of lifestyle, delayed urination, insufficient water intake, and dehydration due to excessive sweat discharge are the trigger factors for urinary tract infection. The typical symptoms are high fever, chills, flank pain, nausea, vomiting, and urination, and in the early stages, it is easy to be confused with cold body aches, so many people miss the right time to treat them. However, if pyelonephritis is left unattended, it can be exacerbated by sepsis, decreased renal function, and chronic renal failure.
Pyelonephritis has a higher incidence of women because the female urethra is shorter than that of men, so bacteria easily penetrate. In addition, diabetics, pregnant women, elderly people, and immunocompromised people are classified as high-risk groups, and high-risk groups require active treatment and treatment even if their symptoms are mild.
Lee Hyo-sang, a kidney specialist at H Plus Yangji Hospital, said, `Shinwoosinitis can often be thought of as a simple urinary tract infection, but if antibiotic treatment is not started quickly due to the spread of bacteria to the actual kidneys, it can develop into sepsis and can be dangerous to life.' The specialist emphasized that "For prevention, proper urination habits such as sufficient water intake, maintenance of cleanliness after urination, and removal of residual urine are important."
Treatment of pyelonephritis usually requires taking antibiotics for 7 to 14 days. Inpatient treatment and intravenous antibiotic administration are required if oral administration is difficult due to high fever and vomiting.
Rarely, if an abscess has been formed, drainage is required as an additional procedure. After treatment, lifestyle correction and detailed examination of urinary system structure abnormalities should be performed when repeated infections occur to prevent recurrence.
The domestic medical community explains that the number of pyelonephritis patients increases during summer and change of seasons. This is because dehydration and lack of water intake due to sweat discharge increase the risk of urinary tract infection. Pyelonephritis can often be considered light, but if left unattended, it is a dangerous disease that even threatens life.
Lee Hyo-sang, a specialist, said "It determines the prognosis to receive diagnosis and treatment early without neglecting even small symptoms", and "In particular, high-risk patients must undergo lifestyle management and regular checkups".
|
This article was translated by Naver AI translator.